Seventy years ago, David Harrington, an ophthalmologist who almost single-handedly put visual fields on the map, authored an article in the American Journal of Ophthalmology on Psychosomatic Interrelationships in which he stated: “Words are to the psychiatrist what the stethoscope is to the cardiologist; and ophthalmologists are notoriously short on words. There is a precision of diagnostic and therapeutic procedure to ophthalmology which has encouraged too accurate particularization and has led to a conspicuous neglect of such evanescent qualities as psychic factors in ocular disease.”

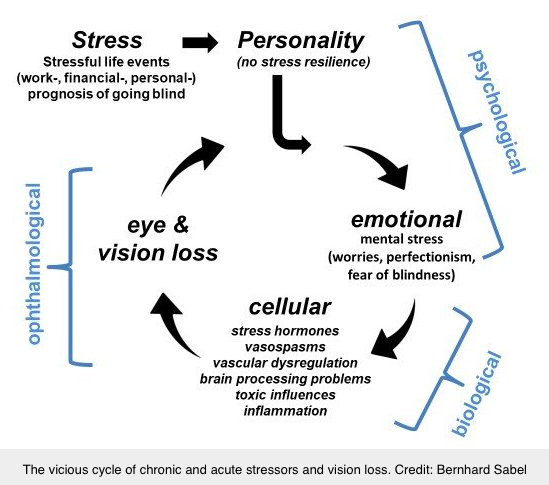
Chances are you’re familiar with the concept of tubular visual fields, which is secondary to stress in conditions such as functional vision loss or Streff Syndrome. But a contemporary approach to visual field loss incorporating psychosomatic medicine is making the news these days, and the “before and after” results for fields pictured above are from the article by Sabel et al titled: Mental stress as consequence and cause of vision loss: the dawn of psychosomatic ophthalmology for preventive and personalized medicine, which provides substantial food for thought. Echoing Harrington’s thoughts, Sabel and colleagues write:
“One might argue sensory functions are purely physiological, i.e., not influenced by the patients’ state of mind. To check if this somato-centric interpretation of vision is unique to ophthalmology, we carried out the same analysis for the sense of hearing for ear (172,353) or hearing loss (78,780). While the scientific output was only about one third of that related to eye and vision, the number of publications of the combined term mental stress hearing loss, was 1.2% (306), i.e., almost double that of vision. In other words, somato-centric thinking not only dominates vision research, but it creates also a negative bias against a role of mental-stress in vision loss.
This low number of scientific records addressing the interface of stress and vision loss dovetails what patients are also complaining about: that there is minimal interest (if any), or even a negative bias against, psychological concerns in the ophthalmology clinical and research community. Yet, there is a rich repertoire of literature on psychological treatments such as stress reduction, relaxation techniques (such as yoga and meditation), cognitive therapies, and psychotherapy. They might be valuable adjuvant methods for a more holistic approach in ophthalmology for treating the person behind the eye.”
Bernhard Sabel’s name may be familiar to you. He was the main proponent of the Vision Restoration Therapy (VRT) device for therapeutic rehabilitation of visual field loss. Sabel earned his Ph.D. in Psychobiology in 1984, and did a two year post-doc at M.I.T. in Neuroanatomy and Neurochemistry. But prior to that he undertook studies in the transfer effects of transcendental meditation (TM). More recently, he has been studying the effects of micro-current stimulation on visual restoration. Sabel and colleagues detailed their holistic approach to vision rehabilitation in this editorial in the Journal of Current Glaucoma Practice .
In the following YouTube video from a meeting in Berlin last November, Sabel presents the principles of his approach to psychosomatic ophthalmology.
Sometimes it seems like it takes forever for ideas to be accepted as mainstream.
At this point, forever is looking comparatively good. 😉
The only one he needs to add to his diagram of disciplines is us. I’m not at all offended, just wish there were a more open and flexible relationship, not so much “us and them.” His presentation was fascinating and the implications of the work he is involved with in changing sick fields has so much to offer patients.
Agreed, Irene! In citations outside of our field we are too often viewed as tag-alongs (or worse) rather than the pioneers we have historically been, for example this blog from a few years ago in which Bernhard Sabel is quoted: https://well.blogs.nytimes.com/2014/05/26/eye-practice-for-the-big-game/
Approximately 20 years ago, Don Getz invited Sabel to present a small group of us during our yearly practice management meeting. That was when he was beginning to market his VRT concept. So I know that he is well aware of our expertise and interest in this area. Twenty years later, I’m still waiting for him to cite Optometry in a publication or presentation. Am I delusional to think that one day we will receive our due accord from Sabel and the general neuro-rehabilitation community? That is, for other professionals to insist that we are an essential member of the patient care therapy team rather than us having to raise our hands and voices to remind them.
👍👍
I would like to refer back to your comment that “forever is looking comparatively good.” I am a bright side kind of person (that may enter my name into the delusional category), maybe 20 years isn’t all that long relative to forever?