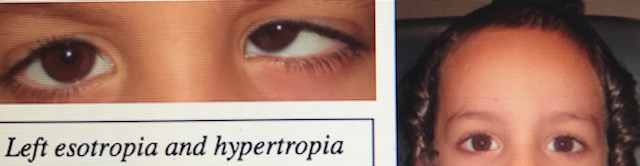
In Part 1 we cited a classic difference of professional opinion between ophthalmology and optometry regarding eye muscle surgery for strabismus. Here’s another case that typifies some of the discussions on VTPU about which parents feel conflicted. This one involves Efraim, a five year-old, who I saw for the first time in my office a couple of weeks ago. There is a strong family history of strabismus, so his parents have been vigilant about his eyes. They reported first noticing that his left eye periodically turning inward and upward last year, and he has considerable disinterest in learning to read. After taking him to the surgeon who operated on his siblings, they received this summary:

So what’s the difference of opinion here?
If a child’s eye turns inward and upward, but doesn’t do so until 3 inches from the the face, he doesn’t have a binocular problem as long as sensory fusion is normal. How do ophthalmologists test sensory fusion in a 5 year-old? Most likely only by their ability to correctly identify the Random Dot E. But does that really provide evidence of sufficient fusion to sustain the demands of near tasks such as reading? The thinking, and this prevalent with every pediatric ophthalmologist I’ve encountered (particularly when the deviation is eso or hyper rather than exo) is that this has no bearing on reading performance unless it occurs constantly as the reading distance.

But recall the parents’ history. They do see the eye periodically turning inward and upward, and they aren’t making this observation at a 3 inch viewing distance! And they are very good historians, and understand when strabismus is present and when it isn’t, given the family history with other siblings. So I would trust the parents’ report in this instance that the strabismus is occurring at some times at the child’s reading distance (which for a 5 year-old is around the 10-12 inch distance). As we know, the variability in fusion often results in more instability and confusion than a constant strabismus in which there is lack of fusion (con-fusion is often more disruptive than no-fusion). They’re not comfortable with the advice to do nothing unless the misalignment becomes bad enough to require strabismus surgery. Low plus, yoked prism, and binasal occlusion might be just what the doctor should order here.
Why not build up fusional ability with ranges?
A noble goal; not likely to happen with this particularly five year old at this point in time. Definitely on the agenda for the future.
Is your present approach stabilization? How often is he to be monitored?
Yes, Michael. Stabilization. To be monitored at a frequency no less than once every three months. I project that he’ll be
developmentally ready to participate more actively in vision therapy within a year’s time.
Dear Lenny,
As previously posted, pediatric ophthalmologists are limited in their understanding of strabismus and its implications on visual, psychological and academic issues. Their model is limited to SURGERY. It is similar to the concept related to a person who has a hammer and can only SEE nails. In this case, the problem is exacerbated by the hyper component, which is not a common variable in visual dysfunctions, which should be ignored. With the parents history and the awareness of a fragile binocular system, the time to intervene is NOW. We are again dealing with a flawed medical and insurance system, which delivers SUB STANDARD CARE to our patients.
Thanks again for another insight into our insane health system. It would seem to rational minds that some intervention is better than no intervention. In this case, ophthalmologist only have one solution, a hammer, excuse me an operation. Thanks again for sharing and teaching your readers that there are alternatives in health care and they need to be pro-active versus being intimidated by a flawed medical system
Richard
Big thumbs up, Richard!!!!
I was wondering if you have a moment how you would use yoked prisms in this case? Thanks!
Sure. The field of maximal inferior oblique elevation is in the adducted position, so a combination of plus and base-in prism is what I would try first (by definition, convergence results in secondary adductive movement of each eye). However, vertical yoked prism is worth probing, as base-down yoked prism can sometimes accomplish similar results because it lessens the action of the superior obliques – that is cases where OAIO is really a secondary over-action associated with excessive innervations to underacting yoked superior obliques.